A Journey Through the VCH Mental Health “System”
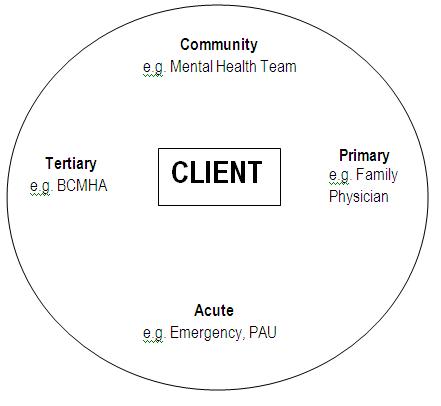
When someone first starts using the VCH mental health and addiction services, they are often understandably confused. Here is an attempt to illustrate it. Let’s imagine Neela, a fictional client, moving in and through mental health/substance use services in Vancouver.
Primary Care – Family Physicians, Counsellors, etc.
Neela has always struggled with depression. When she lost her job, she started drinking heavily again. Her family doctor referred her to an Addiction Counsellor at Evergreen, one of the community health clinics. With that counsellor’s help, Neela decreased her drinking.
“Acute” – Emergency, Psychiatric Assessment Unit, Inpatient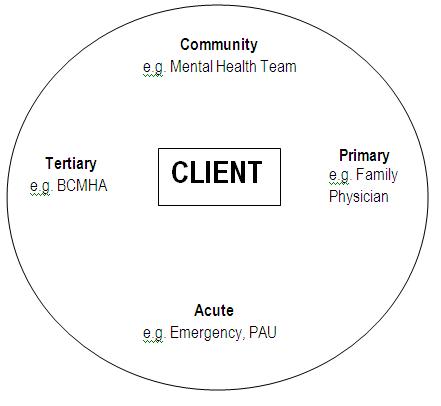
Unfortunately, a year later, her father died. The grief intensified her depression to the point where she tried to take her life. Her spouse, Mary, found her before it was too late, and brought her to VGH. At VGH, they noticed that they had a choice to go to Emergency, or to the new Access and Assessment Center (AAC) just down the street in the Segal building at 803 W. 12th. The AAC deals with urgent mental health matters but in more comfortable surroundings than Emergency. At the AAC, it was established that Neela would be at a high risk of attempting suicide again.
Neela then got admitted at the Psychiatric Assessment Unit in order to stabilize her and to assess what course of treatment would be best to decrease suicide risks and alleviate her depression. PAU is a locked unit where patients typically don’t spend more than five days. Discussing Neela’s history with herself, Mary, and her brother, it turned out that her depression was not only complicated by a long-standing drinking problem but that she also might fit the profile for Bipolar Disorder. PAU usually focuses on an initial (often tentative) diagnosis, on pharmaceutical treatment, and on stabilizing patients so that they are not a threat to themselves or others.
After three days at PAU, Neela is sent to inpatient unit on the 7th floor of the Segal building, one of the four Inpatient units. The 7th floor also often treats people with concurrent disorders (i.e. a mental illness combined with addiction). Inpatient units employ nurses, psychiatrists, psychologists, occupational therapists, etc. People typically stay for one to four weeks. Neela found it easy to trust the psychologist, and more issues came up, such as PTSD due to sexual assault, a medication addiction, and earlier suicide attempts.
“Tertiary” – Longer-Term Residential
Because of the complicated nature of Neela’s mental health and addiction issues, she was referred to the provincial Burnaby Center For Mental Health an Addiction. She lives at BCMHA for six months, working with a fully interdisciplinary team, including art and recreation therapists, mental health workers, nurse practitioners, acupuncturists, etc. BCMHA is a longer-term residential facility; we usually refer to them as “tertiary.” As Neela gets better, she spends more and more time outside of BCMHA, visiting with friends, staying at home overnight, etc.
“Community” – Mental Health Teams and other community resources
Neela participated in treatment in acute and tertiary environments which helped her bring her mental illness to a level that can be managed at home, and which also helped her start on a solid path to recovery from her addictions. Neela and her team accomplished this to a great part because they activated her own strengths, skills and resources, as well as that of her natural support systems.
Neela is now living at home again and is supported by a Mental Health Team. She has a Case Manager there who coordinates assistance for Neela – among others, a psychiatrist and a vocational rehabilitation counselor. Neela is also taking advantage of services in the community, for example a weekly group at the Mood Disorders Association. In the community, Neela also sees primary care practitioners again – her family doctor and addictions counselor.
***
Neela’s journey is only one among many. There are many more services that can help a person improve their mental health. However, hopefully this article makes the VCH mental health & substance use service system just a little easier to understand.