The system & the family
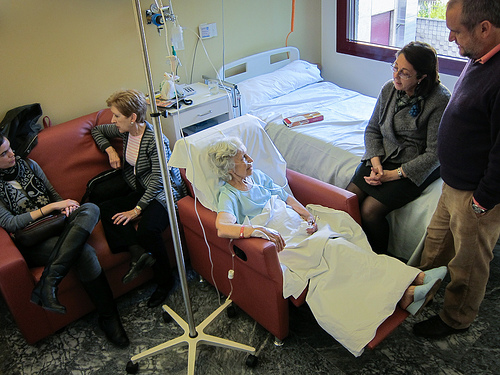
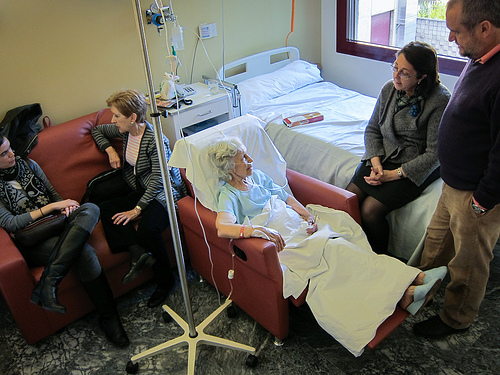 Having recently spent four weeks with my very old mother, who has advanced Parkinsons and dementia, I had an opportunity to think about families from yet another perspective. One of the biggest impressions I came away with was that my mother and our family felt like a very small cog in a very big system. The system was this machine of staff and schedules and rules that kept my mother and her room clean, delivered food and medication, responded to what it perceived as emergencies and – well, mostly it was being a machine. A nice machine, by the way! With very few exceptions, the staff was friendly, the atmosphere in the care home was pleasant, and the food was not too bad.
Having recently spent four weeks with my very old mother, who has advanced Parkinsons and dementia, I had an opportunity to think about families from yet another perspective. One of the biggest impressions I came away with was that my mother and our family felt like a very small cog in a very big system. The system was this machine of staff and schedules and rules that kept my mother and her room clean, delivered food and medication, responded to what it perceived as emergencies and – well, mostly it was being a machine. A nice machine, by the way! With very few exceptions, the staff was friendly, the atmosphere in the care home was pleasant, and the food was not too bad.
However, it felt as if that machine was rolling along inexorably, and anything that deviated from its routine just a bit was something that had to be pushed for. It felt as if the wellbeing of my mother and our family was not its first priority. “Felt” is the right word; it’s actually hard to put my finger on it. When we made requests, asked questions or suggested ideas, nobody rebuffed us; but most of the time it was as if those requests, questions and ideas landed in a place where they would disappear unless we pushed and prodded some more.
Now I’m not saying that everything should be made easy for clients and families. It’s very important to take responsibility, speak up, etc. No question about that. But … and there’s that little but … as a client/patient/consumer and as a family, we are already stressed and vulnerable. We are worried, we are tired, we need to juggle our lives with whatever the health concern is. If there were just a few less things that we had to ask for and think about, we could concentrate more on what we, as mothers, sons or friends can give to our loved one, rather than on being their case manager. And it felt to me as if the system, the “machine”, was most concerned with its needs, rather than the needs of my mother (or even mine).
One example was that we noticed that our mother had not had physiotherapy for nine months. If we at least knew that that’s something we had to check up on we could have done something but because my sister can only visit her in the evenings and on weekends, she never had a chance to notice. Physiotherapy was not part of the cleaning-feeding-medication-emergency management machinery, so it fell between the cracks.
As a family member, is that an experience you have had, as well? Is yours different?
Of course systems aren’t perfect. But then I see it as part of our job here at the Family Team to help make the system a bit better.
I’m not alone with this, by the way. Anne Snowdon from the Ivey International Center for Health Innovation at Western University in London, Ontario wrote a White Paper on “Measuring What Matters – The Cost vs. Values of Health Care” (available at http://sites.ivey.ca/healthinnovation/files/2012/11/White-Paper-Measuring-What-Matters.pdf).
Here are a few excerpts from the report:
Current measures of health system performance focus primarily on access to care, and quality outcomes that identify primarily hospital related adverse events, such as hospital acquired infections, mortality, and readmissions to hospital.
There is no interface between Canadians’ values … and how health services are funded … there are no incentive models or measures used to account for health system outcomes that align with the values of health, wellness, or quality of life for Canadians.
Fortunately, the report says that
Health performance measures are transitioning in Canada from a more traditional model that is health-provider-centric, to one that captures quality outcomes linked more directly to patients. The transition of these performance systems is evolving and will continue to do so over time.
I’d be very interested to hear your thoughts on this. Please feel free to email me at Isabella.Mori@vch.ca, or anyone else at the Family Team.